
Most of us have experienced issues with sleep at various times in our lives. However, if you are having difficulty falling or staying asleep on three or more days a week and these difficulties are causing distress or problems in daily life, then your sleep issues may fall into the category of insomnia. It is estimated that 7-10% of people are affected by insomnia, with resulting health, social, and economic consequences (Ohayon, 2002; Sofi et al., 2014; Daley et al., 2009).
Insomnia is frequently experienced by people with mental health conditions, including depression and anxiety. Approximately 40-55% of people experiencing a psychiatric disorder will also experience insomnia (Harvey, 2001). This has led to the proposal that targeting and treating sleep problems could be an effective way of reducing the severity of co-occurring mental health conditions (Harvey, 2008). Insomnia can often be treated without the use of pharmaceuticals or sleep aids. In fact, psychological treatments for insomnia have demonstrated to produce lasting effects and many patients prefer this approach over a pharmacological one (Espie et al., 2012). To this end, SilverCloud had joined in the fight against insomnia by developing an online Cognitive Behavioral Treatment for Insomnia (CBT-I), known as the Space for Sleep program.
What is Space for Sleep?
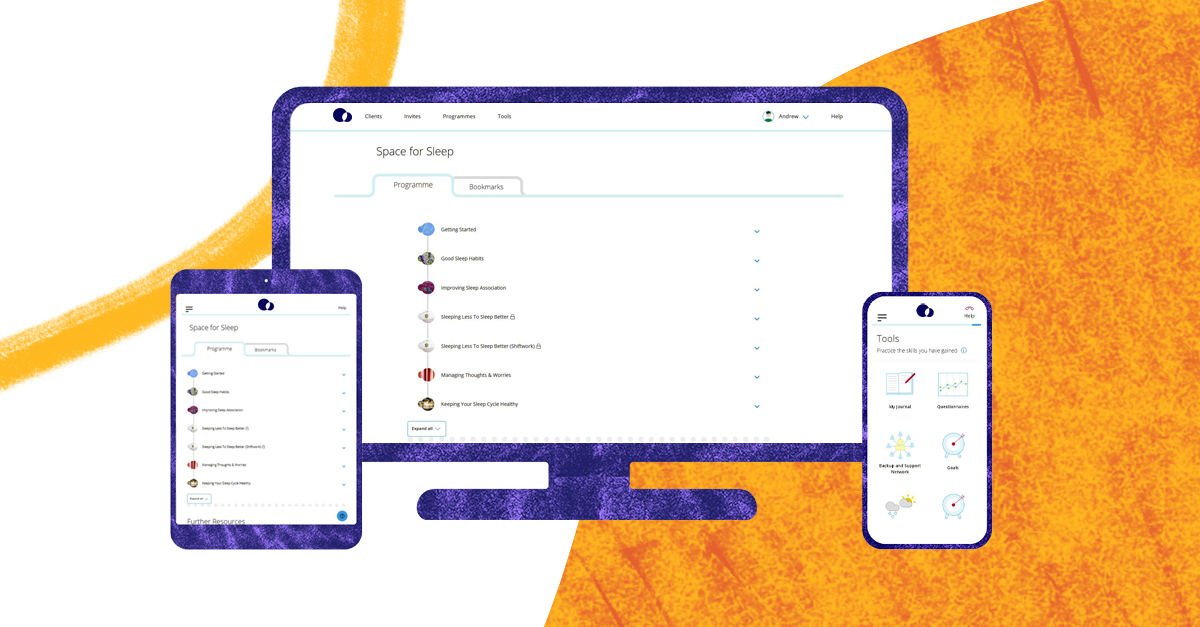
Space for Sleep is an online CBT-I program that aims to improve the symptoms of insomnia through the following five core modules (plus 1 unlockable module):
- Psychoeducation on sleep, insomnia, and CBT-I
- Teaching good sleep habits
- Unlearning negative associations around sleep and bedtime
- Reducing time in bed to primarily sleep time (unlockable module)
- Challenging problematic beliefs and worries about sleep
- How to prevent future relapses
Each module takes roughly 40-60 minutes to complete and the user is encouraged to try one module per week. Typically, a mental health coach will support the user on their journey through the program, with regular check-ins to review their progress and offer guidance. The coach can tailor the program to better suit the needs of the user, for instance a module dealing with sleep restriction can be unlocked for the user, if it is deemed relevant. The modules follow a robust structure, incorporating videos, informative content, quizzes, interactive activities, as well as homework suggestions and summaries. Throughout their use of the program users are encouraged to keep a sleep diary to monitor the amount and quality of their sleep, and to reflect on the impact the program is having on their daily life.
As well as developing online treatments, a critical part of SilverCloud’s mission is to continually and scientifically evaluate if these treatments are effective. SilverCloud recently conducted a study examining the effectiveness and user satisfaction of Space for Sleep. This study has recently been published in the scientific journal Internet Interventions (Wogan et al., 2021).
Study findings
In the study, participants were recruited from an Improving Access to Psychological Therapies (IAPT) provider within the United Kingdom’s National Health System. IAPT providers utilize a stepped care model in which mental health concerns are categorized based on severity and receive treatment based on one of five steps of increasingly intense treatment. Online mental health treatments, such as those offered by SilverCloud Health, are classified as a “Step 2” service for people with mild to moderate depression or anxiety. Study participants were enrolled in Space for Sleep if they had mild to moderate symptoms of depression or anxiety and reported difficulties falling or staying asleep for at least three months. Participants were assigned an online coach for support throughout their engagement with the program. During treatment, participants reported on their insomnia symptoms, mental health, day-to-day functioning, and program satisfaction.
Key results indicated that users of Space for Sleep reported a decrease in their symptoms of insomnia over time, as well as an improvement in their mental health and day-to-day functioning. User satisfaction with the program was also high with approximately 80-90% of users reporting that the program was supportive, relevant, interesting, and helpful. Platform usage metrics demonstrated that on average, participants spent 4 weeks on the program, during which they logged in 16 times and spent 4.5 hours engaging with the content.
In sum, this study suggests that Space for Sleep reduced insomnia symptoms while providing a relatively brief, satisfying, and supportive experience to its users. While these results provide promising findings for Space for Sleep, an important limitation of these findings is the lack of a control group in the study, that is a lack of a group that can be used to compare changes in insomnia symptoms for those enrolled in Space for Sleep to the changes in insomnia symptoms for those who were not in treatment. This is a key limitation that SilverCloud Health aims to address in future research. The study also laid the groundwork for identifying and planning ways the program itself could be further developed and optimized.
Future plans for Space for Sleep – Program Optimization
When developing programs SilverCloud follows an agile methodology, continually iterating and refining content based on user feedback (from both clinicians and participants), even after release. The ongoing development of the Space from Sleep program will adhere to this methodology, incorporating recommendations made by the recent study and addressing the most common issues raised in user feedback. These future program optimizations will focus on the following key areas:
1. Increased coach training on the clinical management of insomnia.
A more in-depth training on how coaches can best guide patients with insomnia symptoms through the digital program will be developed. More specifically, the coach training will consist of improving understanding of insomnia symptoms, validated assessments, and program tools as well as making sure to only discharge users when their insomnia symptoms have improved substantially.
2. Increased user engagement with the sleep diary tool
A core tool threaded throughout the program is the Sleep Diary. The more the user engages with this tool, the more likely they will be to get the full benefit of the program by being able to recognize and measure changes in their sleeping patterns over time. Feedback from coaches has highlighted the need to emphasize the importance of using this tool in the program content so that the user is encouraged to develop a habit of filling in their sleep diary, almost from the day they start using the program. Adaptations to the functionality of the tool will assist users in being able to quickly input data from their previous night’s sleep.
3. Increase program impact by unlocking the sleep restriction module for everyone
The concept of sleep restriction is introduced in the 4th module. Sleep restriction is a technique that is highly effective over time at reducing difficulties falling asleep and staying asleep. However, this module is not currently part of the core program content and can only be seen by users if it is unlocked by the user’s coach. Study results implicate that all users should be able to access this module, so the product team will review the program content and structure to ensure that there are no possible risks in making the module part of the core content and reordering it so that it appears earlier in the program.
Conclusion
Insomnia is a prevalent sleep disorder that carries significant personal and societal consequences. Results from the current study indicate that Space for Sleep shows promise as an effective tool for combating insomnia and reducing these consequences. Because SilverCloud Health is committed to providing highly effective evidence-based treatments, SilverCloud Health aims to further develop the Space for Sleep program and its scientific support by continuing to develop and optimize the content and interactive elements of the program as well as conduct further rigorous examinations of the effectiveness of the program. SilverClould Health looks forward to helping people overcome insomnia by providing an easily accessible, first-line insomnia treatment that is supported by robust scientific evidence.

Authors:  Garrett Hisler is a Clinical Research Associate at SilverCloud Health and has a PhD in Social/Personality Psychology from Iowa State University. His background and research has largely focused on how sleep and circadian rhythms interface with personality processes, self-control, and technology use. Leveraging this background, he hopes to utilize digital modalities of mental health treatments to more widely help people connect with and improve their sleep and mental health.
Garrett Hisler is a Clinical Research Associate at SilverCloud Health and has a PhD in Social/Personality Psychology from Iowa State University. His background and research has largely focused on how sleep and circadian rhythms interface with personality processes, self-control, and technology use. Leveraging this background, he hopes to utilize digital modalities of mental health treatments to more widely help people connect with and improve their sleep and mental health.
 Niamh Conolly is the Content Lead in SilverCloud Health and has an MSc in Interactive Digital Media from Trinity College Dublin. She specializes in digital content strategy, finding ways to manage and leverage content. In SilverCloud Niamh works with cross-functional clinical and development teams to produce online mental health programs which are accessible to a range of audiences.
Niamh Conolly is the Content Lead in SilverCloud Health and has an MSc in Interactive Digital Media from Trinity College Dublin. She specializes in digital content strategy, finding ways to manage and leverage content. In SilverCloud Niamh works with cross-functional clinical and development teams to produce online mental health programs which are accessible to a range of audiences.
References
Daley, M., Morin, C. M., LeBlanc, M., Grégoire, J. P., & Savard, J. (2009). The economic burden of insomnia: Direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Sleep, 32, 55-64.
Espie, C. A., Barrie, L. M., & Forgan, G. S. (2012). Comparative investigation of the psychophysiologic and idiopathic insomnia disorder phenotypes: Psychologic characteristics, patients' perspectives, and implications for clinical management. Sleep, 35, 385-393.
Harvey, A. G. (2001). Insomnia: symptom or diagnosis? Clinical Psychology Review, 21, 1037-1059.
Harvey, A. G. (2008). Insomnia, psychiatric disorders, and the transdiagnostic perspective. Current Directions in Psychological Science, 17, 299-303.
Ohayon, M. M. (2002). Epidemiology of insomnia: What we know and what we still need to learn. Sleep Medicine Reviews, 6, 97-111.
Sofi, F., Cesari, F., Casini, A., Macchi, C., Abbate, R., & Gensini, G. F. (2014). Insomnia and risk of cardiovascular disease: A meta-analysis. European Journal of Preventive Cardiology, 21, 57-64.
Wogan, R., Enrique, A., Adegoke, A., Earley, C., Sollesse, S., Gale, S., ... & Richards, D. (2021). Internet-delivered CBT intervention (Space for Sleep) for insomnia in a routine care setting: Results from an open pilot study. Internet interventions, 26, 100443.







